A New Era of AI in connected healthcare: Shifting the healthcare paradigm
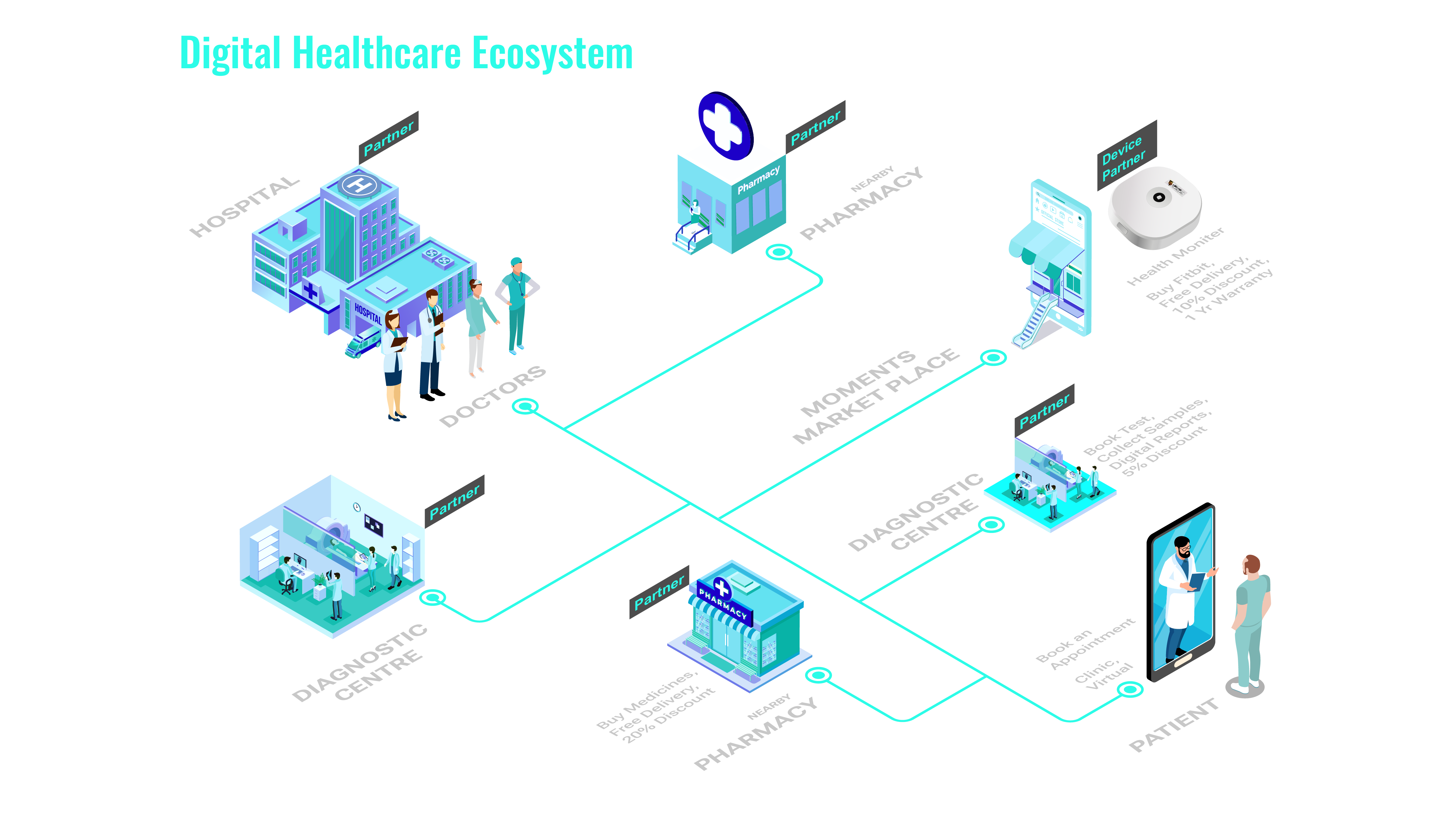
Artificial Intelligence (AI) has revolutionized healthcare, delivering proactive care to enhance health outcomes, and streamline processes while reducing costs. At its core healthcare is driven by data - vital signs of a patient, their clinical data, medical history, diagnoses, medications, treatment plan, and test results. Imagine this data flowing seamlessly between various specialists in the healthcare ecosystem, who can leverage this data for their timely expertise. This transformation holds the power to revolutionize patient care and optimize the efficiency of the complete healthcare ecosystem. This change is brought about through better connectivity and transparent sharing of data and insights across health insurers, hospitals, clinics, and retail pharmacies.

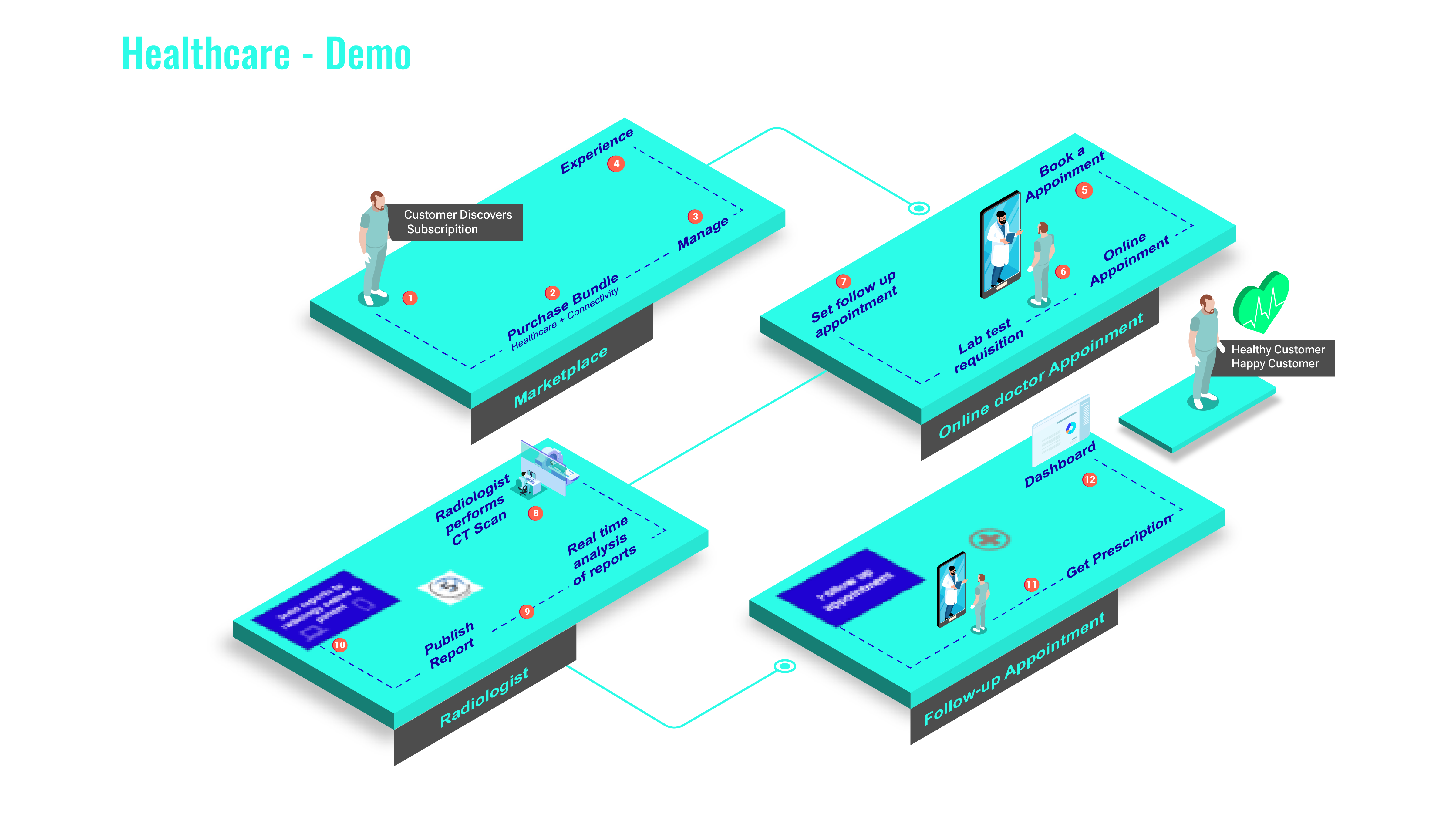
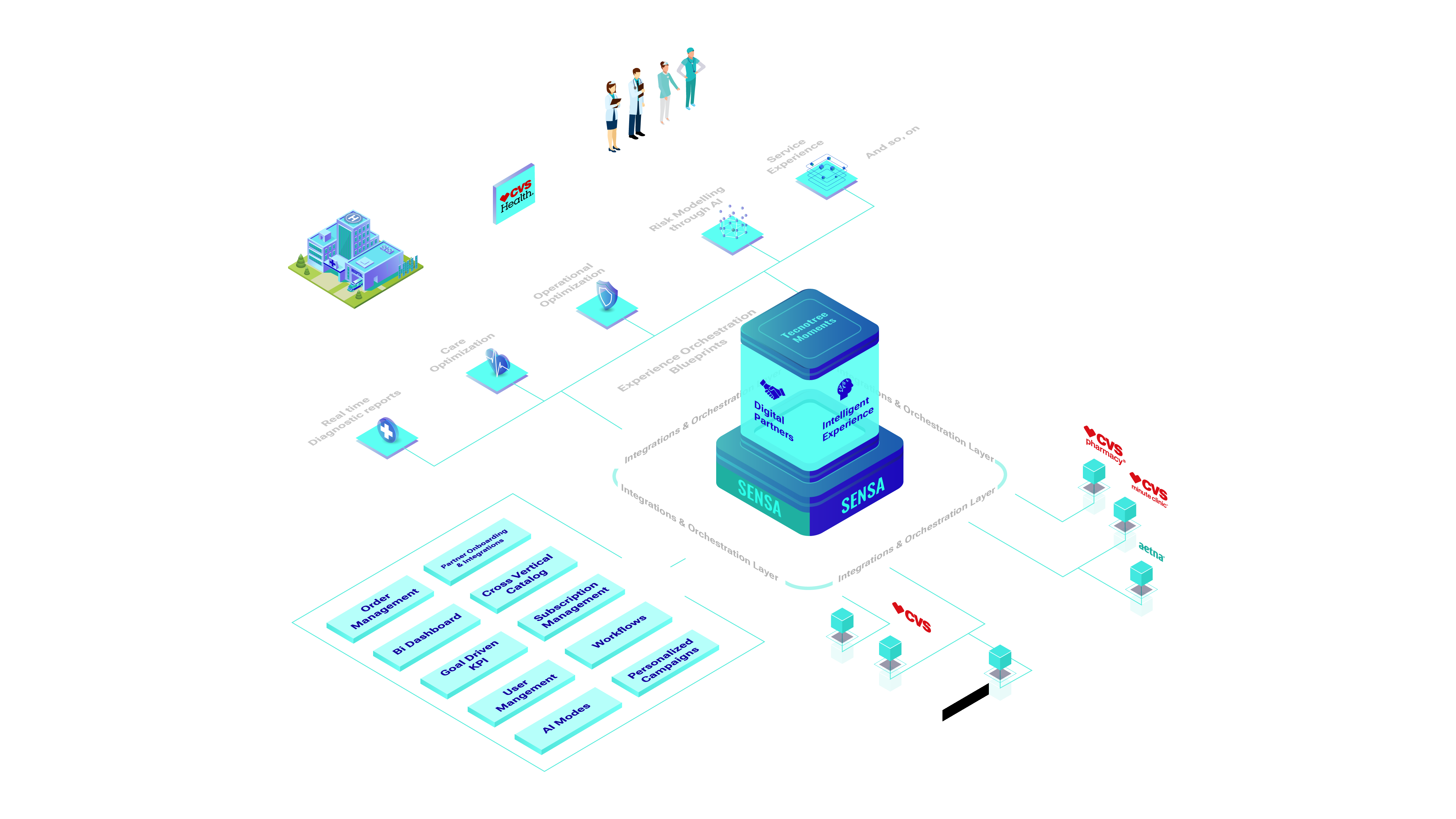
B2B2X healthcare platform - Connected health ecosystem for B2B2X experiences is poised to revolutionize healthcare through:

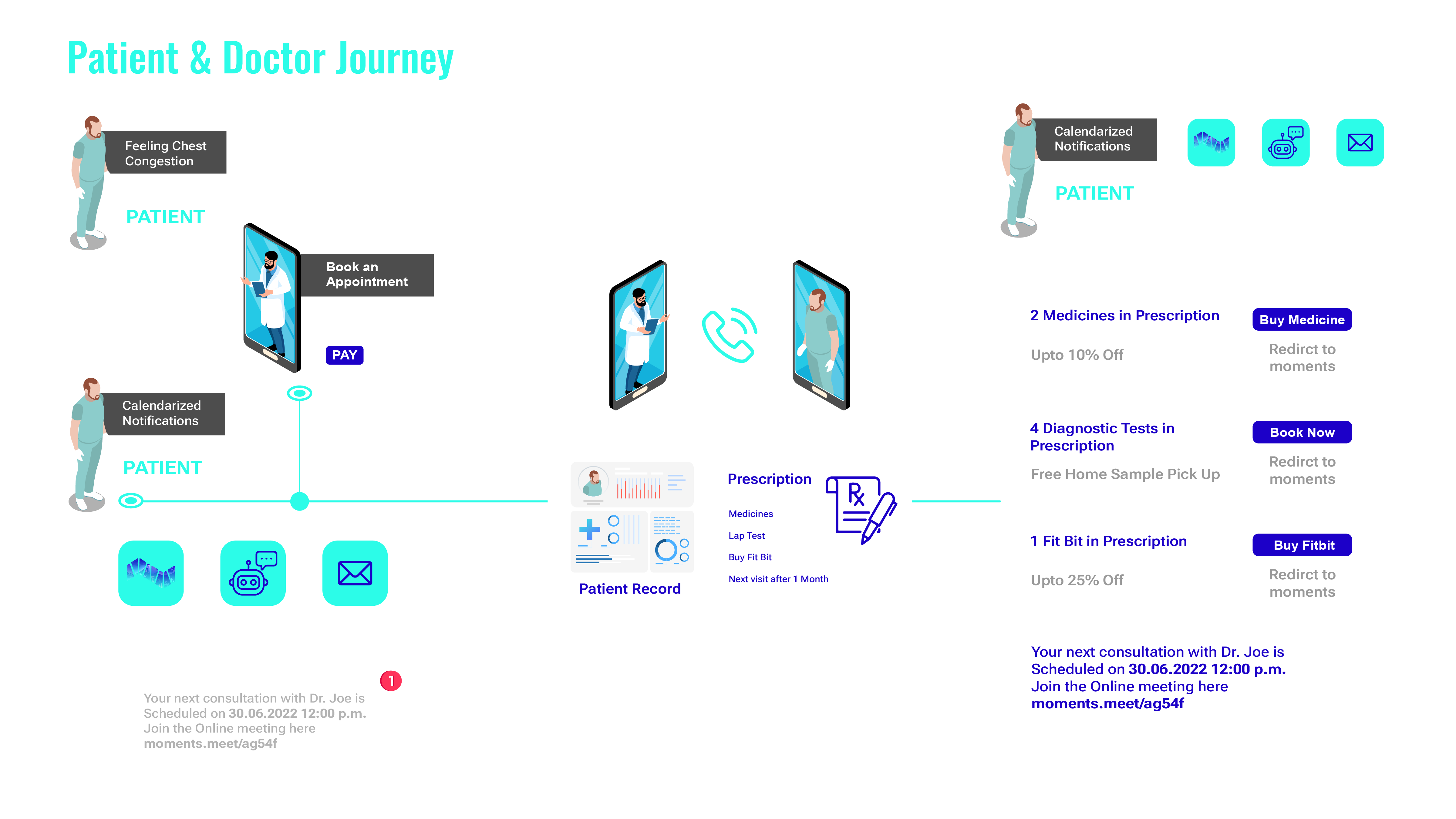
Multi-experience virtual care and AI based diagnosis and intervention

A low-code no-code enterprise self-service platform for healthcare providers for automated workflows and interoperability between partners
Multi-experience Orchestration Through 5G network optimization & Al Enablement
- 20,000 + international doctors ready for consultation
- 12+ Acuity Care device integrations for Tele ICU
- 7+ loT devices for remote care onboarded
- 300+ Al disease intervention blueprints
Discover Our Solutions
Platforms capabilities/ Healthcare Offerings
Use Cases
Healthcare AI Solutions
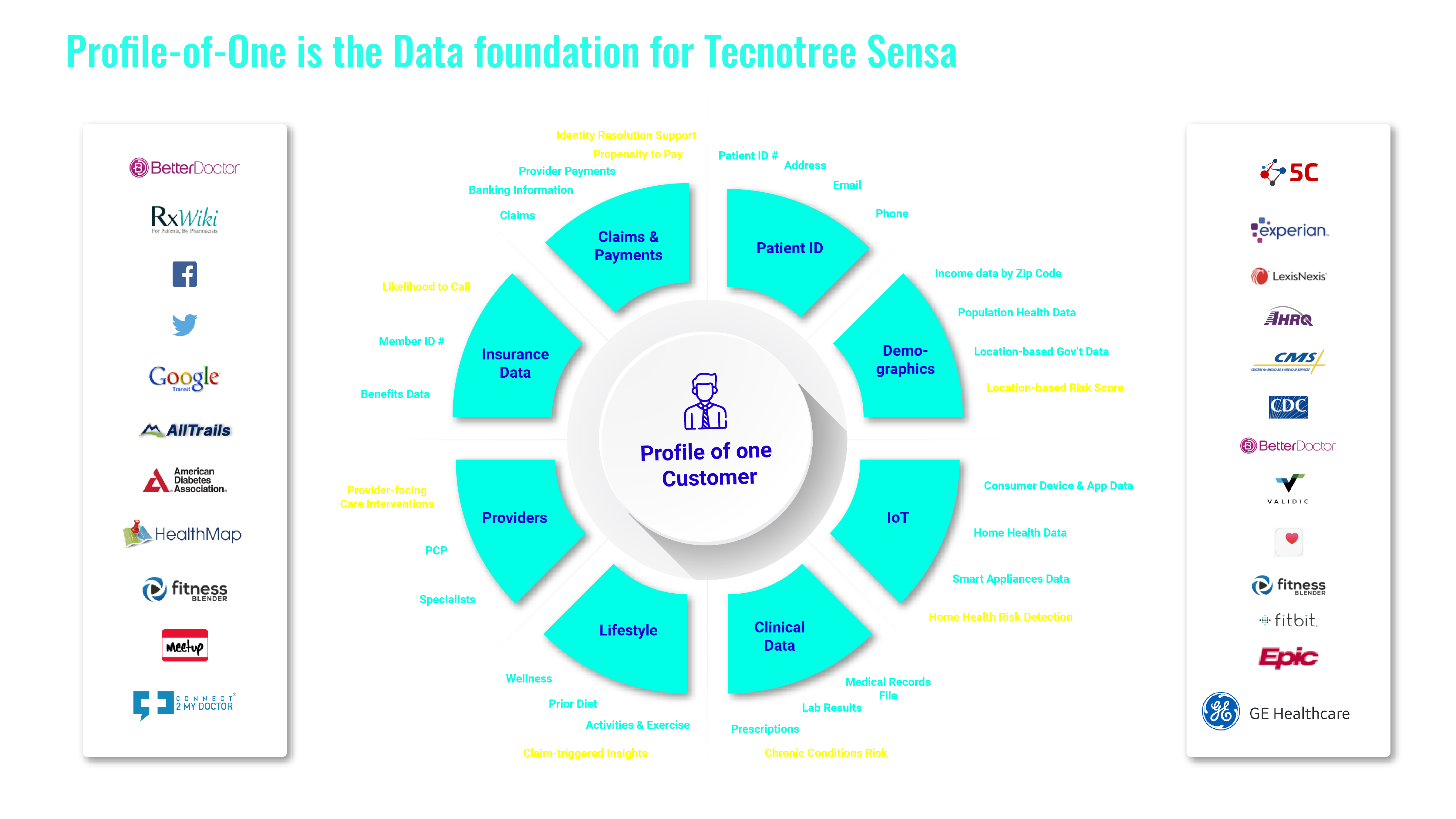
- Personalized, Predictive, Proactive Care & Service
- Engineer better patient outcomes while lowering costs through predictive and proactive personalized care.
- Patient and Member profiles form a key foundation for personalized insights and proactive interventions.
- We Know Healthcare AI
- Healthcare AI Personalization
- Leverage Patient, Member, Provider and Claim Profiles
- 360 Degree Perspective
Healthcare-specific AI-powered solutions and products that accelerate Member and Patient engagement in the following areas:
Care Optimization
- High-cost Claims
- Care Interventions
- Star Rating Improvements
Patient / Member Experience
- Chatbot
- Self Service
- Agent Assist
- Intelligent Call Routing
Sales Acceleration
- Intelligent Lead Gen
- Plan Match
- Medicare Conversion
Combine enterprise-wide data collection with external data to enrich profiles and the customer experience. Tecnotree’s foundational Profile-of-One technology gives you a 360-degree view of an entity like a person (patient, member, provider) or claim, using Declared, Observed and Inferred data to drive hyper-personalized insights.
Case Studies
Annual cost savings in contact center operations
Improvement in contact center agent satisfaction
Reduction in average handle time on calls
Annual liability prevention costs saved
Models scanned
Impacted patients for discharge
Increase in number of quality leads
Annual marketing spend reduced
Improved lead conversion
6 Use cases in progress and 12+ on 2022 - 2023 roadmap
Annual savings from member experience disruption use case
Annualized savings from initial CKD pilot